Key Takeaways:
- Bariatric surgery leads to type 2 diabetes remission in the majority of patients, with many experiencing improvements in blood sugar levels before significant weight loss occurs.
- Different procedures have varying effectiveness for type 2 diabetes, with gastric bypass showing the highest remission rates.
- Long-term studies suggest that bariatric surgery lowers the risk of cardiovascular events and other serious conditions in people with type 2 diabetes.
If you're living with type 2 diabetes and struggling with excess weight, you've probably tried countless diets, exercise plans, and medications. The constant blood sugar monitoring, medication adjustments, and worries about long-term complications can be quite taxing. That's why many people turn to bariatric surgery as a potential solution for both their weight and diabetes.
But is bariatric surgery for diabetes really the "ultimate fix"? We're going to explore this question together, breaking down the science and looking at what this option might mean for you or someone you care about.
[/box]
Link Between Obesity and Type 2 Diabetes
Before diving into bariatric surgery, it's important to understand why obesity and diabetes are so closely connected.
The Weight-Diabetes Connection
Did you know that if you're carrying extra weight, you are at a greater risk of developing type 2 diabetes? Even being moderately overweight increases your risk.
The good news is that addressing your weight can have a profoundly positive impact on your diabetes. Even losing just 10–15 pounds can make a significant difference.
Think about it this way: for many people, excess weight and diabetes are like two sides of the same coin. When you tackle one, you often improve the other. That's why weight loss is usually one of the first things doctors recommend when you're diagnosed with type 2 diabetes.
How Excess Weight Affects Your Insulin
Your body produces a hormone called insulin. This acts like a key that unlocks your cells, allowing sugar (glucose) to enter, where it is used for energy. But when you have excess body fat, especially around your midsection, something frustrating happens—your cells start ignoring insulin.
This is called insulin resistance. Your pancreas tries to compensate by pumping out more insulin, but eventually, it can't keep up. Sugar builds up in your bloodstream instead of entering your cells, and type 2 diabetes develops.
So, if insulin is the key, obesity makes your body change the locks, so the key doesn't work as well anymore. Your pancreas has to produce more and more insulin to open the same number of cells. Eventually, the key factory (your pancreas) gets exhausted and can't produce enough working keys.
What many people don't realize is that by the time you're diagnosed with type 2 diabetes, this process has usually been happening in your body for years. Your pancreas has been working overtime, and your cells have been growing increasingly resistant to insulin's effects.
The Inflammation Factor
Another piece of the puzzle is inflammation. Excess fat tissue isn't just sitting there—it's actually actively releasing chemicals that cause chronic inflammation throughout your body. This inflammation disrupts your body's insulin signaling pathways, making insulin resistance even worse.
Scientists have discovered that fat cells, particularly those located around the abdomen, release inflammatory substances known as cytokines. These cytokines interfere with the body's normal response to insulin. So, not only is the body requiring more insulin due to insulin resistance, but inflammation is also actively disrupting the insulin that is present, preventing it from doing its job properly.
This vicious cycle is one of the reasons why diabetes can be so difficult to manage with lifestyle changes alone once it's established. The inflammation and insulin resistance feed off each other, creating a challenging situation for your body to resolve without significant intervention.
How Bariatric Surgery Impacts Diabetes
Now, let's discuss the remarkable impact of bariatric surgery on diabetes. For many people, the results can seem almost miraculous. Bariatric surgery for diabetes is increasingly recognized not only for its role in managing blood sugar but also for addressing other obesity-related health concerns. For example, some studies also explore bariatric surgery for hypertension, showing improvements in blood pressure alongside glycemic control.
Diabetes Improvement or Remission
One of the most exciting things about bariatric surgery and type 2 diabetes is the possibility of remission—meaning your blood sugar levels return to normal without medication. Studies show that up to 74% of patients experience diabetes remission within two years after gastric bypass surgery.
This has led many to ask, “Does bariatric surgery cure diabetes?” While the term “cure” is debated, remission is certainly achievable, especially when weight loss is sustained and healthy lifestyle changes are maintained.
Even more surprisingly, many patients notice improvements in their blood sugar levels within two weeks after surgery, before they've lost significant weight. This suggests that the surgery is accomplishing something beyond just aiding in weight loss.
What exactly is remission? Medical professionals typically define diabetes remission as:
- Having an A1C below 6.5%
- Not needing diabetes medications
- Maintaining these results for at least one year
Some patients achieve "complete remission," characterized by normal blood sugar levels and no medication for 5 years or more. Others experience "partial remission," characterized by improved blood sugar levels and a reduction in medication needs. Either way, the improvements can be life-changing.

The possibility of putting diabetes into remission is what makes bariatric surgery for type 2 diabetes such an attractive option for many people.
Better Blood Sugar Control
Even if complete remission doesn't occur, most patients achieve much better control of their diabetes after surgery. Hemoglobin A1C levels (the test that shows your average blood sugar over three months) often drop significantly.
The effect of bariatric surgery on diabetes control typically outperforms what can be achieved with intensive medical therapy and lifestyle changes alone. Many patients who struggled for years to keep their blood sugar in check find it much easier after surgery.
Better control means more than just improved numbers on lab tests. It translates to:
- More energy and less fatigue
- Fewer instances of low or high blood sugar
- Reduced risk of diabetes complications like heart disease, kidney problems, and nerve damage
- Better overall quality of life
For someone who has been riding the blood sugar rollercoaster for years, this newfound stability can be an incredible relief.
Reduced Need for Medications
After bariatric surgery, many patients find they need fewer diabetes medications—or none at all. This reduction in medication needs usually happens quickly and continues as weight loss progresses.
Many patients report that one of the most satisfying aspects of their post-surgery experience is watching their medication list shrink. Some people who were taking insulin plus multiple oral medications find themselves medication-free within weeks or months. Even those who still need some medication usually require much lower doses.
This reduction in medication dependency can have positive ripple effects throughout your life, from fewer side effects to more flexibility in your daily routine and significant cost savings over time.
Types of Bariatric Surgery and Their Effectiveness for Diabetes
Not all weight loss surgeries are equal when it comes to improving diabetic symptoms. Here's a breakdown of the main types and how they compare for diabetes treatment:
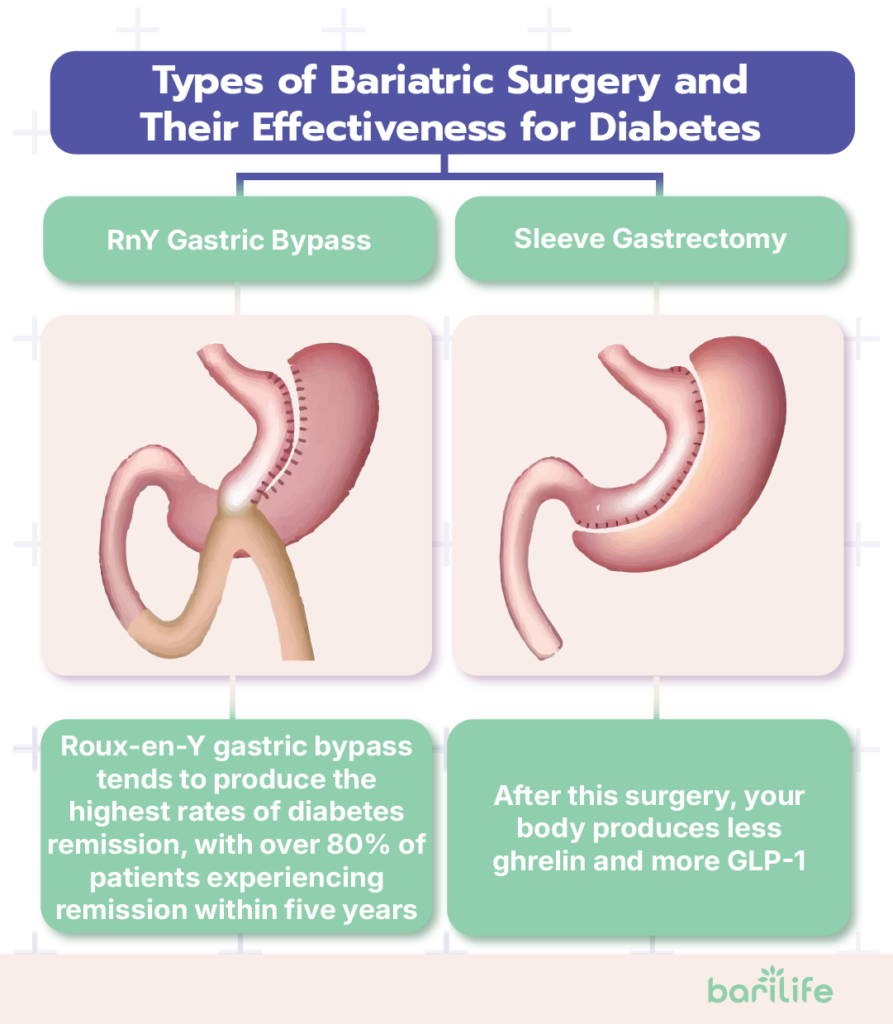
Roux-en-Y Gastric Bypass
This procedure, often considered the "gold standard" of bariatric surgery and diabetes management, works in two ways:
- The surgeon creates a small pouch at the top part of your stomach, dramatically reducing the amount of food you can eat.
- This pouch is connected directly to the mid-portion of your smaller intestine, bypassing the rest of your stomach and the first section of your small intestine.
Roux-en-Y gastric bypass tends to produce the highest rates of diabetes remission, with over 80% of patients experiencing remission within five years.
Why is gastric bypass so effective for diabetes? Scientists believe this is due to changes in gut hormones and the gut microbiome—the bacteria that reside in the digestive system. The surgery changes the way your body processes food and the signals it sends to regulate blood sugar.
Sleeve Gastrectomy
This increasingly popular procedure involves removing approximately 80% of the stomach, leaving a sleeve-shaped pouch that is significantly smaller than the original stomach. While less complex than gastric bypass, it remains highly effective in managing diabetes.
The sleeve primarily works by restricting food intake and altering gut hormones. After this surgery, your body produces less ghrelin (the "hunger hormone") and more GLP-1 (a hormone that helps regulate blood sugar).
Due to its more straightforward technique and excellent results, sleeve gastrectomy has become the most popular type of bariatric surgery in the United States. For many patients with diabetes and obesity, it offers a good balance of effectiveness and reduced surgical complexity.
Adjustable Gastric Banding
This procedure involves putting an inflatable band around the upper part of your stomach, making a small pouch above the band. The band can be adjusted over time, making it loose or tight, by adding or removing saline through a port that's placed under your skin.

When it comes to bariatric surgery for type 2 diabetes, gastric banding tends to be less effective than other procedures. Diabetes remission rates are about 30-45%. The improvements also tend to happen more slowly, primarily as weight loss occurs.
Unlike bypass or sleeve procedures, banding doesn't significantly change gut hormones or metabolism independent of weight loss. This may explain why its effects on diabetes are less dramatic and more directly tied to the amount of weight lost.
Due to its lower effectiveness for diabetes remission and higher rate of long-term complications, gastric banding has declined in popularity in recent years.
Emerging Procedures
Research continues on newer procedures that may offer benefits for diabetes while being less invasive. These include:
- Duodenal-jejunal bypass liner: A flexible tube that lines the first part of your small intestine, mimicking some effects of gastric bypass without permanent changes
- Endoscopic sleeve gastroplasty: Creating a sleeve-like restriction in the stomach using sutures placed with an endoscope (no external incisions)
- Gastric balloon: A temporary balloon placed in the stomach to create feelings of fullness
While these approaches show promise, they generally don't match the effectiveness of traditional bariatric surgeries for diabetes remission. However, they may offer options for patients who aren't candidates for more invasive procedures or who prefer a less permanent intervention.
Long-Term Outcomes and Considerations
If you're considering bariatric surgery for diabetes management, you may be wondering about the long-term results. Will the improvements last? What should you be prepared for down the road?
Sustained Weight Loss
One key to improving diabetes after surgery is maintaining sustained weight loss. Most patients lose about 60-80% of their excess weight 12 to 18 months post-surgery.
While some weight regain is common after the initial loss (typically about 5-10% of body weight), most patients maintain significant weight loss in the long term. This sustained weight loss helps keep diabetes under control.
Studies following patients for 10 years or more show that most maintain enough weight loss to continue experiencing health benefits, even if they do not maintain their lowest weight. This long-term success rate is significantly higher than that achieved with non-surgical weight loss methods.
For diabetes management, even partial weight loss maintenance can make a big difference. Research suggests that losing just 5-10% of your body weight can improve insulin sensitivi

Leave a Comment
Your email address will not be published.