The internet can be a jungle of information, with much of it being unreliable or lacking scientific evidence to back it up. That’s why figuring out which weight loss surgery is the safest can be quite confusing. Rest assured you have landed in the right place because we are going to break down the pros and cons of the major weight loss surgeries here.
What is bariatric surgery?
Bariatric surgery, also referred to as weight loss surgery, is an umbrella term that describes any surgery that alters the digestive tract in order to bring about weight loss. The surgery itself varies as some may reduce the size of the stomach or change the shape of the small intestine.
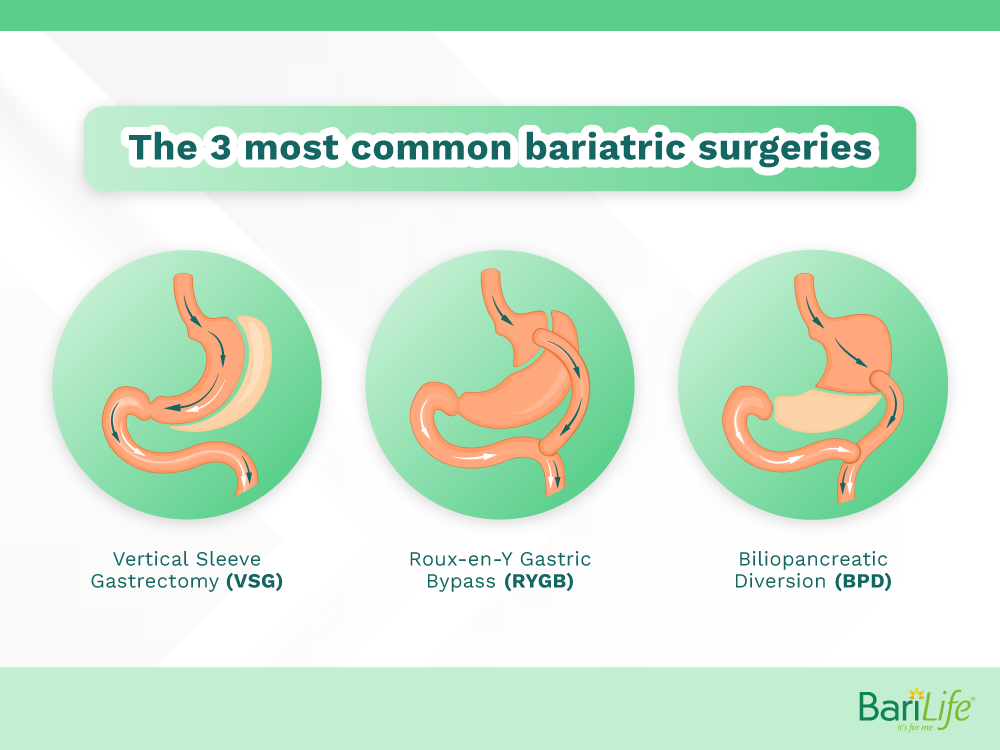
The three most common bariatric surgeries that you may have heard of include gastric bypass, gastric sleeve, and duodenal switch. Each procedure is unique and comes with its own set of risks and benefits.
Is bariatric surgery safe?
As with any surgery, there are risks associated with bariatric surgery. We will go into specifics for each surgery in a bit. However, research shows the complication rate for bariatric surgery, in general, is quite low at about 1.4%, with a 0.04% mortality rate. Of course, that wasn’t always the case. In the late 1990s, these rates were much higher with complications topping out at about 11%, and approximately 1% of all that underwent the procedure did not survive.
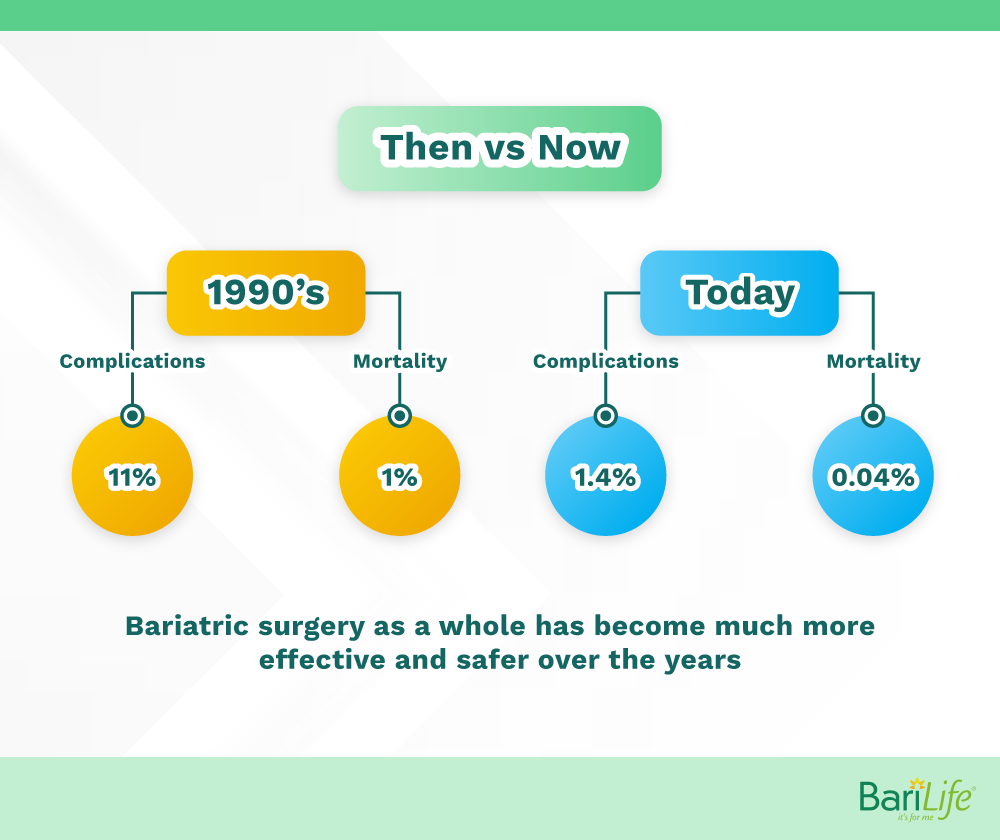
Thankfully, technology and experience have greatly improved the safety of bariatric surgery over the years. Most surgeons would agree that these surgeries are now considered very safe.
What are the different types of bariatric surgery?
The different types of bariatric surgeries include:
Gastric bypass
During a gastric bypass, the surgeon creates a small pouch out of the top portion of the stomach. This pouch then “bypasses” the remaining part of the stomach and the upper part of the small intestine, and is then connected further down on the small intestine.
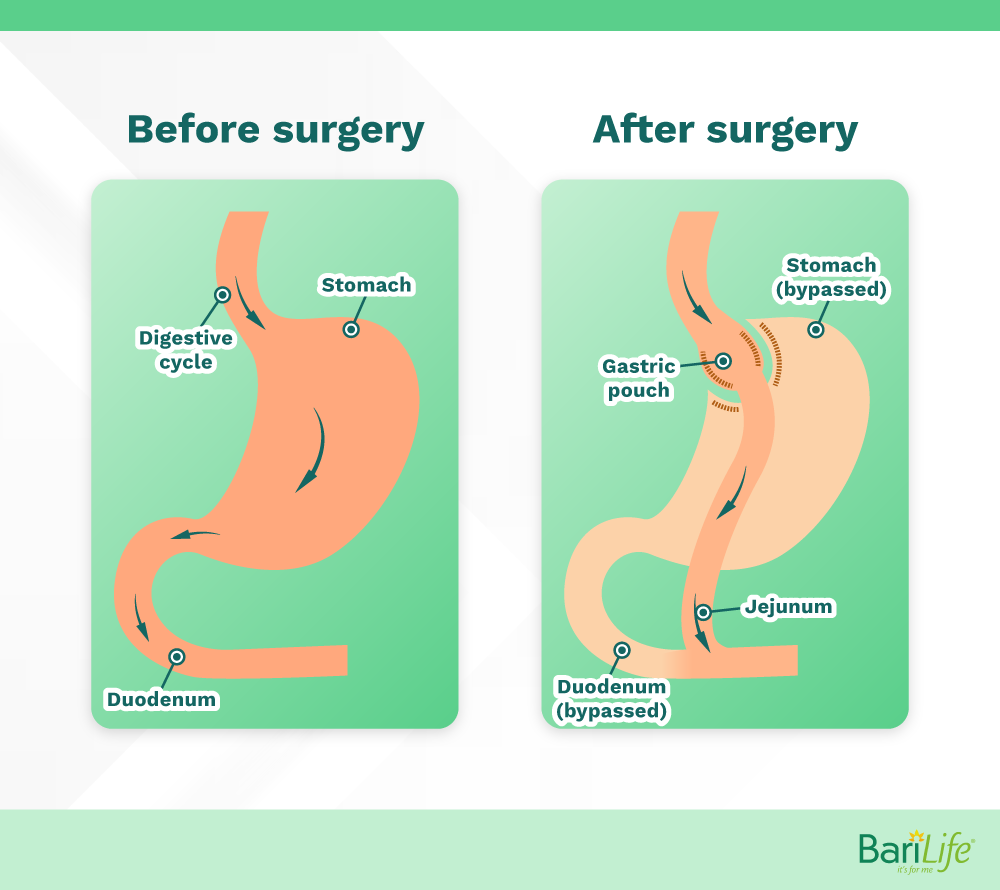
The new small stomach that is created by the surgeon will allow the patient to feel full more quickly, allowing the individual to eat less. Because part of the small intestine is bypassed, calories and nutrients cannot be absorbed as they normally would. This leads to an additional reduction in overall calories taken in due to what is referred to as, malabsorption.
Gastric sleeve
Also referred to as the sleeve gastrectomy, the gastric sleeve procedure removes a significant portion of the stomach, leaving a small tube, or “sleeve” left. The intestines are not altered during this surgery, therefore, not requiring the bypass of any portion of the digestive tract.
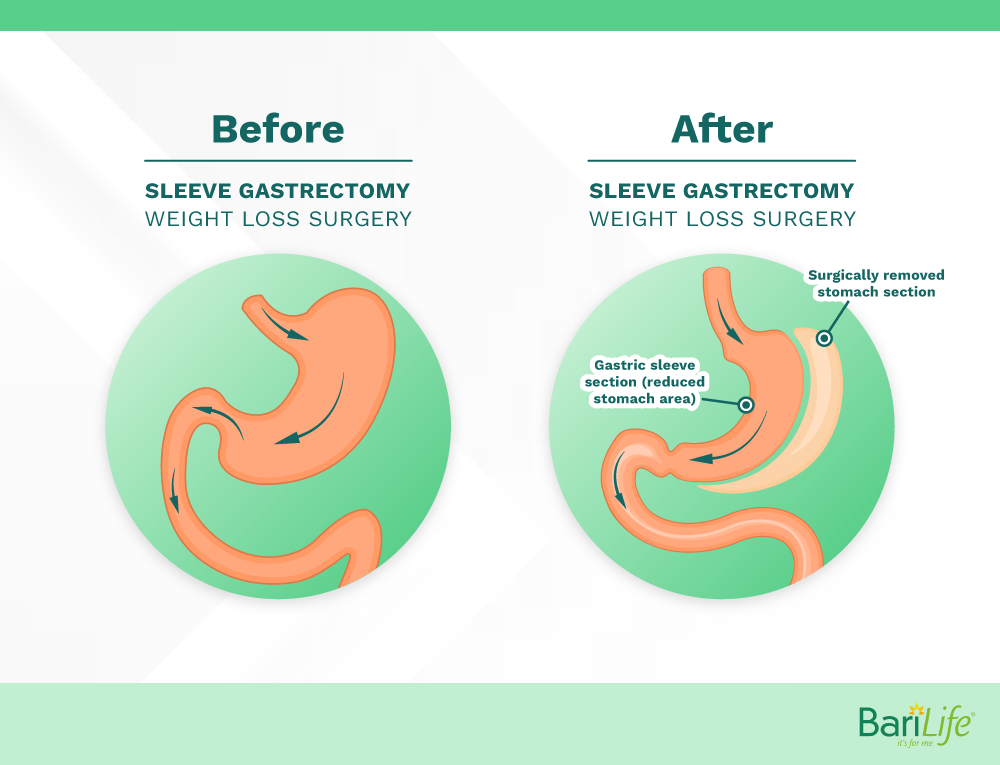
Similar to the first part of the gastric bypass, the stomach is made much smaller and therefore, an individual will not be able to eat nearly as much because they will feel full more quickly. Because the small intestine remains intact, malabsorption of calories and nutrients does not take place.
Duodenal switch
The duodenal switch procedure begins as a gastric sleeve, in which the majority of the stomach is removed, leaving a sleeve-shaped tube. Then the upper portion of the small intestine is temporarily removed and the lower part of the small intestine is brought up and connected a little below the stomach.
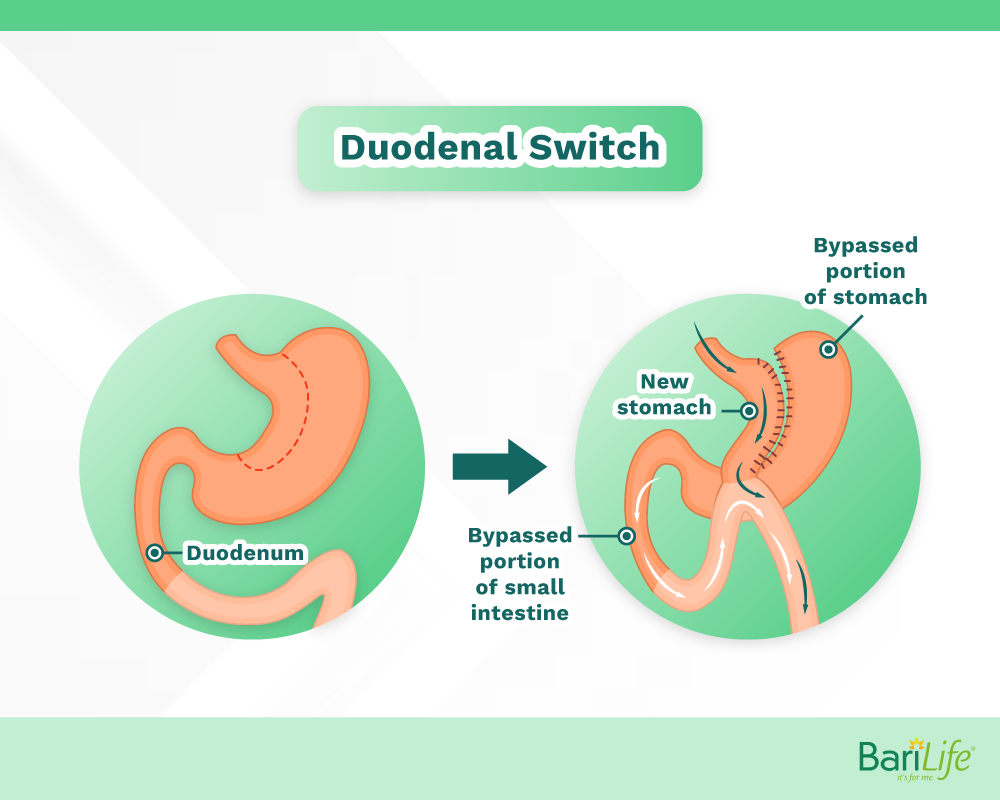
The intestine that was removed is then reconnected to the top and lower portion of the small intestine with the sole purpose of allowing enzymes to mix with food prior to reaching the colon.
It is important to mention that the muscle that controls stomach emptying at the bottom of the stomach, called the pylorus, is preserved. This will decrease some unwanted side effects – more on that soon. The small, sleeve-like pouch allows the patient to feel full with less food.
Because the food will not have contact with the upper portion of the small intestine, malabsorption will occur. That is when calories and nutrients from food cannot be absorbed. This leads to an additional decrease in overall daily calories taken in.
Lap-band
This once-popular procedure occurs when the surgeon places a silicone band around the stomach, creating a small pouch in one portion of the stomach. This small stomach pouch should allow the individual to feel fuller longer.
However, due to a variety of complications and a large reversal rate, between 20 and 34%, the lap band procedure has been somewhat disregarded by the bariatric community. For this reason, we won’t discuss this operation further.
Gastric Bypass
| Pros | Cons |
|---|---|
| Weight loss can be 60-80% in the short term, and most maintain a weight loss of 50% excess body weight long term. | Malabsorption can lead to long term nutrient deficiencies |
| Because stomach size is reduced, it simply cannot hold much food | Very involved procedure which can have increased complications when compared to gastric sleeve |
| Hormonal changes can cause an increased daily calorie burn | Irreversible procedure |
| The smaller stomach will allow for increased satisfaction after eating and less hunger between meals | Dumping syndrome is common* |
| Because part of the small intestine is bypassed, food cannot be absorbed as usual, thus leading to even fewer calories taken in throughout the day. | Often requires a longer hospital stay |
| Improvement and resolution in other chronic conditions such as type 2 diabetes, high blood pressure, high cholesterol, and chronic sleep apnea |
*Dumping syndrome occurs after some gastrointestinal surgeries when certain foods, usually high in sugar, cause the stomach to release, or “dump,” stomach contents into the small intestine. This causes a variety of symptoms ranging from uncontrolled diarrhea to palpitations and sweating.
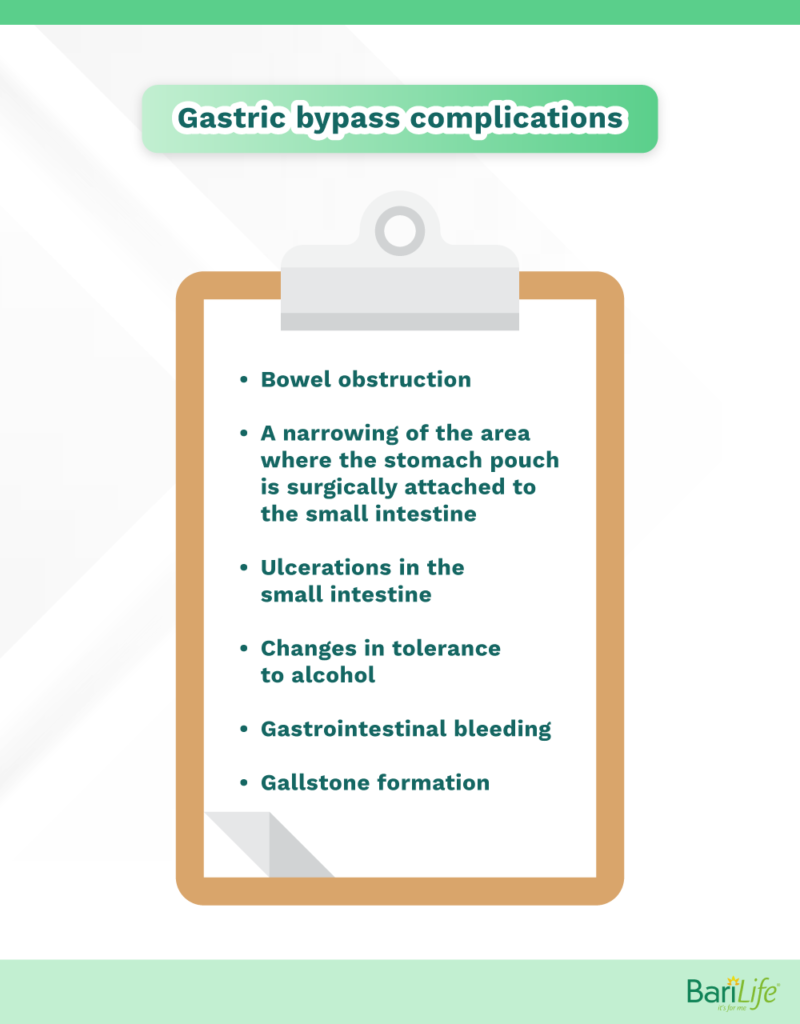
Some gastric bypass complications include:
- Bowel obstruction
- A narrowing of the area where the stomach pouch is surgically attached to the small intestine
- Ulcerations in the small intestine
- Changes in tolerance to alcohol
- Gastrointestinal bleeding
- Gallstone formation
Gastric Sleeve
| Pros | Cons |
|---|---|
| Average weight loss is about 50%, and most are able to maintain weight 3-5 years out | Decreased food volume can lead to long term vitamin and nutrient deficiencies |
| Because stomach size is reduced, it simply cannot hold much food | Irreversible surgery |
| A shorter hospital stay is likely | Risk of complications associated with surgery |
| The smaller stomach will allow for increased satisfaction after eating and less hunger between meals | Higher chance of complications in the early stages after surgery when compared to gastric bypass |
| Improvement and resolution in other chronic conditions such as type 2 diabetes, high blood pressure, high cholesterol, and chronic sleep apnea |
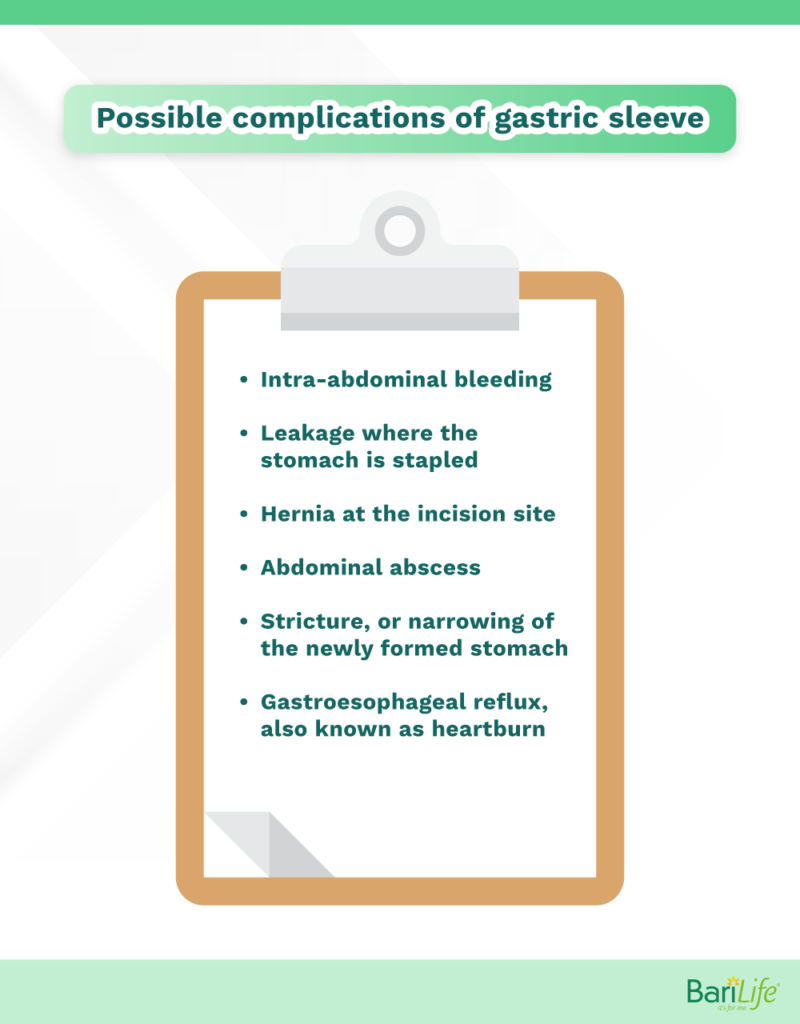
Some gastric sleeve complications include:
- Intra-abdominal bleeding
- Leakage where the stomach was stapled
- Hernia at the incision site
- Abdominal abscess
- Stricture, or narrowing of the newly formed stomach
- Gastroesophageal reflux, also known as heartburn
Duodenal Switch
| Pros | Cons |
|---|---|
| Average excess weight loss is about 69% at 36 months post op | Malabsorption can lead to long term nutrient deficiencies |
| Most sustained weight loss compared to other forms of bariatric surgery | Very involved procedure which can have increased complications when compared to gastric sleeve and gastric bypass |
| Because stomach size is reduced, it simply cannot hold much food | Irreversible procedure |
| The smaller stomach will allow for increased satisfaction after eating and less hunger between meals | Often requires a longer hospital stay |
| Dumping syndrome is less common when compared to gastric bypass | |
| Because part of the small intestine is bypassed, food cannot be absorbed as usual, thus leading to even fewer calories taken in throughout the day. | |
| Thought to be a good revision operation when others have gone wrong. | |
| Improvement and resolution in other chronic conditions such as type 2 diabetes, high blood pressure, high cholesterol, and chronic sleep apnea. Most effective at completely resolving diabetes. |
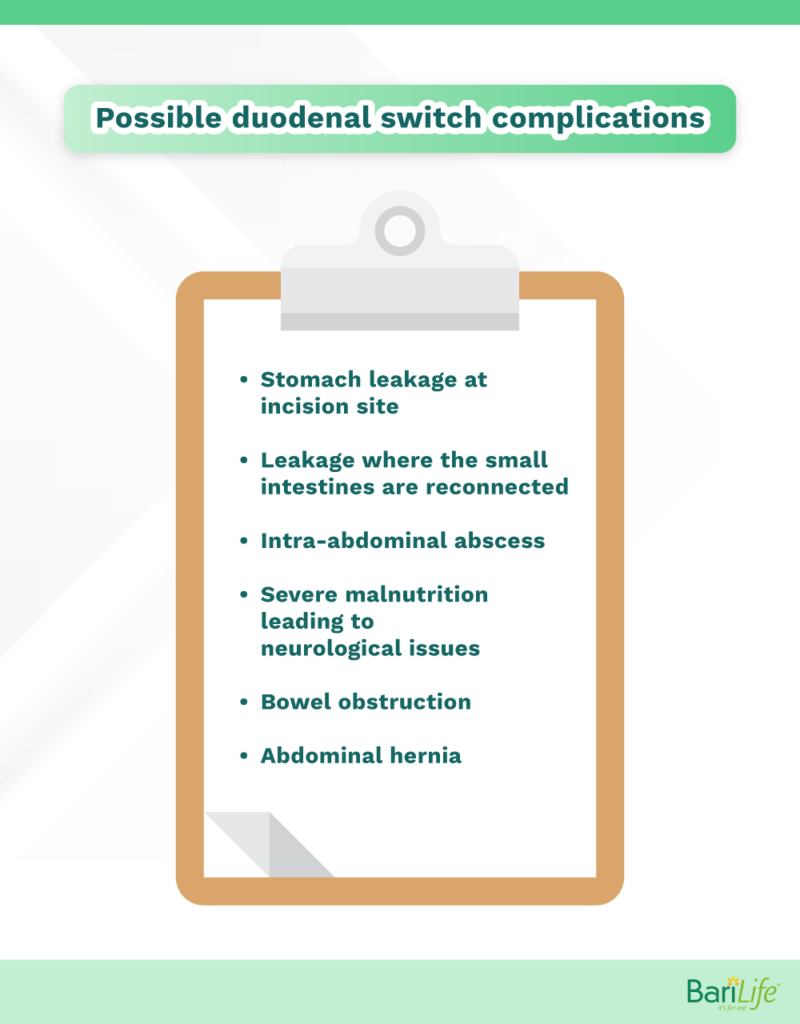
Some duodenal switch complications include:
- Stomach leakage at the incision site
- Leakage where the small intestines are reconnected
- Intra-abdominal abscess
- Severe malnutrition leading neurological disorders
- Bowel obstruction
- Abdominal hernia
Putting it all together
As you can see, each of these procedures has a great track record for overall weight loss success. Having the pros and cons laid out helps us to compare. Let’s take a closer look.
Two of the procedures, the gastric bypass, and duodenal switch, alter the structure of the intestines allowing for malabsorption of calories and nutrients. This is intended to be an added benefit as the individual’s overall calorie intake is decreased throughout the day. However, it can also lead to nutrient deficiencies so it is important to ensure all doctor’s instructions are followed.
Gastric sleeve surgery, on the other hand, only alters the shape of the stomach and does not change the intestinal anatomy. This avoids the risk of severe nutrient deficiencies from malabsorption but also allows more calories to be absorbed. Because the stomach size is reduced in all three surgeries, the individual will only be able to eat small amounts regardless of the surgery performed.
They will feel more full and satisfied with these smaller portions. Eating very small amounts over a long period of time can also lead to nutrient deficiencies, so it is always a good idea to follow recommendations and maintain all required follow-up appointments.
The duodenal switch has the most sustained weight loss compared to the other surgeries. It is also very intricate and comes with the possibility of more complications. The gastric sleeve surgery is a less intricate procedure and therefore has fewer long-term complications, and likely a shorter hospital stay. However, it also is reported to have a slightly lower average weight loss, although still satisfactory.
These are all factors that require thought and discussion before determining what is the safest weight loss surgery.
Which bariatric surgery is safest for you?
As you can see, each of the big three weight-loss surgeries comes with advantages and some disadvantages. When deciding which weight loss procedure is safest for you, it is important to discuss all options with your surgeon and your support team. Your surgeon will take into account your age, activity level, lifestyle, excess body weight, and then offer a recommendation tailored to your specific needs.
By learning about the potential complications of each of the surgeries, you are not only arming yourself with knowledge but also gathering information to ask your surgeon about. Bariatric surgery is not a one-size-fits-all surgery. Work closely with your doctor to determine the surgery that is best for you.



What are your tips and tricks to post-bariatric success?