Key Takeaways:
- Gastric bypass surgery is generally the most effective bariatric option for patients with obesity-related GERD, significantly improving or resolving symptoms in the majority of cases.
- Sleeve gastrectomy, while popular for weight loss, carries a high risk of causing or worsening GERD symptoms, making it a less ideal choice for patients with preexisting reflux.
- A thorough pre-surgery evaluation is crucial to determine the best bariatric procedure and to optimize outcomes for patients struggling with both obesity and GERD.
For many people who struggle with both excess weight and gastroesophageal reflux disease (GERD), the question of whether bariatric surgery can help with both issues comes up.
Some procedures can significantly improve reflux symptoms, while others may actually exacerbate them. Let’s look at what you need to know if you’re considering getting bariatric surgery to help with excess weight and GERD.
Table of Contents
GERD and Its Causes
Before discussing surgical solutions, it’s helpful to understand what happens in your body when you experience acid reflux.
What’s Going Wrong?
At the junction where your esophagus (food pipe) meets your stomach, there’s a muscle ring called the lower esophageal sphincter (LES). This muscle is supposed to act like a one-way valve, allowing food to pass down into your stomach but preventing the contents inside from flowing back up.
When you have GERD, this valve isn’t working properly. It may be too weak, or it might relax when it shouldn’t, making stomach acid splash back into your esophagus. This acid can agitate the delicate lining of your esophagus, causing that familiar burning sensation and other uncomfortable symptoms.
Why Is This Happening to You?
Several factors can contribute to GERD, but excess weight is one of the biggest culprits. Here are other possible factors:
- Smoking (which weakens the LES)
- Certain foods and drinks (like coffee, alcohol, spicy or fatty foods)
- Eating large meals
- Lying down too soon after eating
- Pregnancy
- Some medications
The Hiatal Hernia Connection
Many people with GERD also have what’s called a hiatal hernia. This happens when part of your stomach pushes upward through the diaphragm (the muscle that separates your chest from your abdomen) into your chest cavity.
Normally, your diaphragm helps reinforce your LES, providing an extra barrier against reflux. When you have a hiatal hernia, this support is compromised, making acid reflux more likely. Excess weight increases the likelihood of developing a hiatal hernia, creating a vicious cycle that worsens GERD symptoms.
Implications of Bariatric Surgery on GERD
When it comes to bariatric surgery for GERD, not all procedures provide the same benefits. Some can dramatically improve your reflux symptoms, while others might actually make them worse.
Different Procedures, Different Outcomes
Let’s break down the differences between each surgery.
Roux-en-Y Gastric Bypass
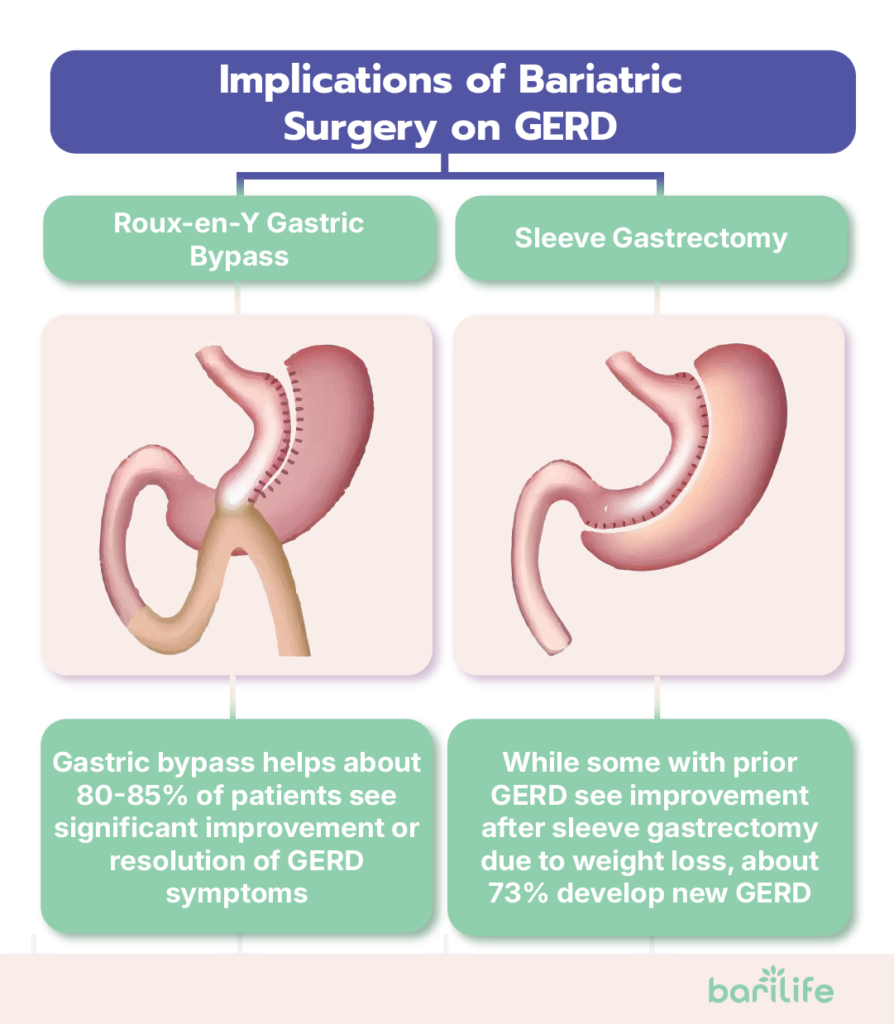
This procedure is generally considered the gold standard for treating obesity-related GERD. It works well because it creates a small stomach pouch that produces less acid. Food bypasses part of the small intestine, reducing bile reflux. The restructured digestive tract makes it physically difficult for acid to travel back up into the esophagus. Weight loss also reduces pressure on the stomach.
Studies show that about 80-85% of patients experience significant improvement or complete resolution of their GERD symptoms after gastric bypass.
In addition to GERD, it has shown positive results for bariatric surgery for hypertension and managing bariatric surgery and diabetes, with some studies exploring whether does bariatric surgery cure diabetes entirely or simply improves glycemic control.
Sleeve Gastrectomy
This increasingly popular procedure has a more complicated relationship with GERD. During a sleeve gastrectomy, about 80% of your stomach is removed, creating a banana-shaped “sleeve.”
The impact of acid reflux after sleeve gastrectomy is mixed. For some patients who had GERD before surgery, symptoms improve as they lose weight. However, about 73% of patients develop new GERD symptoms after sleeve surgery (called “de novo GERD”).
Adjustable Gastric Banding
This procedure, which puts an adjustable band at the upper portion of the stomach, has fallen out of favor in recent years.
When it comes to GERD, the results are mixed and often temporary. While initial weight loss may improve symptoms, many patients experience a return or worsening of GERD over time as the band creates pressure on the stomach.
The Importance of Pre-Surgery Evaluation
Because GERD and bariatric surgery have such a complex relationship, it’s important that your surgical team thoroughly evaluate your reflux symptoms before deciding which procedure might be best for you.
If you have severe GERD, especially with complications like Barrett’s esophagus, your surgeon might strongly recommend gastric bypass over sleeve gastrectomy, even if you initially preferred the sleeve procedure.
Ideal Candidates for Bariatric Surgery to Treat GERD
Who would benefit most from considering bariatric surgery for GERD treatment? Several factors come into play.

When Traditional GERD Treatments Aren’t Working
You might be an ideal candidate if:
- You’ve been diagnosed with both obesity and GERD
- Medications aren’t adequately controlling your reflux symptoms
- You’ve tried lifestyle changes (elevating the head of your bed, avoiding trigger foods, not eating before bedtime) without sufficient relief
- You’re dependent on daily acid-suppressing medications like proton pump inhibitors (PPIs)
- You’re concerned about the long-term effects of either chronic GERD or long-term medication use
Long-standing, uncontrolled GERD can lead to serious complications, including esophageal strictures, Barrett’s esophagus, and even esophageal cancer. If you’re at risk for these complications and also qualify for weight loss surgery, addressing both issues with one intervention could be beneficial.
Weight Considerations
Generally, bariatric surgery is for people with:
- BMI of 40 or higher, or
- BMI between 35 and 40, along with obesity-related health conditions (including severe GERD)
- In some cases, a BMI between 30 and 35 with difficult-to-control GERD might be considered
Looking at the Whole Picture
Your surgical team will also consider:
- Your overall health and other medical conditions
- Previous attempts at weight loss
- Your understanding of the lifestyle commitment required after surgery
- Your dedication to long-term follow-up care
While GERD and bariatric surgery outcomes can be highly positive for the right candidate, these procedures are not simple solutions—they require significant lifestyle changes and ongoing care to achieve optimal results.
Preoperative Evaluations for GERD
If you’re considering bariatric surgery and have GERD symptoms, you’ll need several specialized evaluations to help determine the best approach.
Looking Inside: Upper Endoscopy
Most bariatric surgery candidates with GERD symptoms will undergo an upper endoscopy, also known as an EGD. During this procedure, a thin, flexible tube with a camera is passed down your throat to check your esophagus, stomach, and the first part of your small intestine.
This test is important because it can:
- Assess the severity of any esophageal inflammation
- Check for complications like Barrett’s esophagus
- Identify hiatal hernias
- Rule out other health conditions that could be causing similar symptoms
- Document any abnormalities that might affect surgical planning
If you have severe inflammation or Barrett’s esophagus, your surgeon might be more likely to recommend gastric bypass over sleeve gastrectomy due to its better outcomes for GERD.
Testing How Things Move: Esophageal Manometry
Some patients may also undergo esophageal manometry, which assesses the function of the muscles in the esophagus, including the strength of the lower esophageal sphincter (LES). A small tube is passed through your nose into your esophagus, and you’ll be asked to swallow while the pressure of your esophageal muscles is measured.
This test helps determine if your GERD is related to muscle dysfunction and provides information about how your esophagus might handle the changes created by different bariatric procedures.
Measuring Acid Exposure: pH Monitoring
Another valuable test is 24-hour pH monitoring, which measures the amount of acid refluxing into your esophagus over the course of a day. A small sensor is temporarily placed in your lower esophagus, either with a thin tube through your nose or a small capsule attached to your esophageal wall.
This test can help confirm that your symptoms are truly related to acid reflux and quantify how severe the reflux is. It’s particularly useful if your symptoms are atypical or if there’s any question about whether GERD is the cause of your discomfort.
Evaluating Hiatal Hernias
Since hiatal hernias often contribute to GERD, your medical team will carefully assess whether you have one and how large it is. This might be done through the endoscopy mentioned above or with additional imaging studies.
If a hiatal hernia is identified, your surgeon will likely repair it during your bariatric procedure, which can significantly improve your GERD symptoms regardless of which weight loss surgery you undergo.
Risks and Complications of Bariatric Surgery for GERD
While bariatric surgery can offer significant benefits for GERD, it is essential to understand the potential risks and complications associated with it.
Procedure-Specific GERD Risks
As we’ve discussed, some procedures carry specific GERD-related risks:
Sleeve Gastrectomy
The primary concern with sleeve gastrectomy is the potential for new-onset GERD after surgery.
For patients who already have GERD, the risk of worsening symptoms is something to consider carefully. This doesn’t mean you can’t choose a sleeve procedure if you have GERD, but you should discuss this risk thoroughly with your surgical team.
Gastric Bypass
While generally good for GERD, gastric bypass carries its own set of potential complications, including:
- Marginal ulcers (ulcers that develop at the connection between the stomach pouch and the small intestine)
- Bile reflux (a different type of reflux that can cause symptoms similar to acid reflux)
- Dumping syndrome (rapid emptying of contents in the stomach into the small intestine)
General Surgical Risks
Like any major surgery, bariatric procedures carry risks such as:
- Bleeding
- Infection
- Blood clots
- Adverse reactions to anesthesia
- Leaks from the surgical connections
- Strictures (narrowing) of surgical connections
- Nutritional deficiencies
When GERD Persists or Returns
Even after successful bariatric surgery, some patients may experience persistent or recurrent GERD symptoms. This can happen for several reasons:
- Weight regain puts renewed pressure on the stomach and LES
- A hiatal hernia recurs or wasn’t adequately repaired during surgery
- The new stomach anatomy changes over time
- Dietary choices contribute to ongoing reflux
If GERD persists after bariatric surgery, additional treatments may be necessary, ranging from medication to possible revisional surgery in severe cases.
Post-Surgery Lifestyle and GERD Management
Your actions after surgery play a huge role in managing both your weight and GERD symptoms. Here’s how to maximize your results:
Eating Habits That Help
After bariatric surgery, you’ll naturally need to make significant changes to how and what you eat. Many of these changes also benefit GERD management.
Focus on eating small, frequent meals. Your smaller stomach pouch will require smaller meals anyway, which is also better for GERD, as large meals can increase pressure and reflux.
Eat slowly and chew thoroughly. This aids proper digestion and reduces the chance of discomfort with your new anatomy.
Avoid GERD trigger foods such as:
- Spicy foods
- Acidic foods (citrus, tomatoes)
- Fatty or fried foods
- Chocolate
- Mint
- Coffee and caffeinated beverages
- Alcohol
- Carbonated drinks
Lastly, avoid eating within 2-3 hours of bedtime to reduce nighttime reflux.
Weight Management for GERD Control
Maintaining weight loss is one of the most important factors in managing GERD after bariatric surgery. Focus on following your nutritional guidelines, engaging in regular physical activity, attending all follow-up appointments, and addressing any emotional or psychological factors that might contribute to eating behaviors.
Positioning and Posture
Simple adjustments can make a huge difference in managing GERD symptoms. Consider elevating the top part of your bed by 6-8 inches (using blocks under the bed posts, not just extra pillows).
Avoid lying down immediately after meals and practice good posture when sitting to reduce pressure on your abdomen.
Medication Management
If you were taking medications for GERD before surgery, don’t stop them abruptly without your doctor’s guidance. Talk to your healthcare provider about how your medication needs might change after surgery.
Regular Follow-Up
Ongoing care is essential for monitoring your weight loss and GERD symptoms. Make sure that you attend all your scheduled follow-up appointments. Report to your medical team immediately if you have any new or worsening reflux symptoms. If you had severe GERD before surgery, you might also want to consider getting a periodic endoscopy.
Conclusion
Bariatric surgery for GERD can be life-changing for the right candidates. For many people struggling with both obesity and persistent acid reflux, surgery offers a path to improvement that medication alone can’t achieve.
If you’re considering bariatric surgery and GERD is a significant concern, have a detailed conversation with your healthcare team about how different procedures might affect your symptoms.
While the surgery itself is important, your commitment to the necessary lifestyle changes will ultimately determine your long-term success in managing both your weight and your GERD symptoms.
How Bari Life Can Help
Proper nutrition after bariatric surgery is crucial for both maintaining weight and managing GERD. Bari Life offers a complete range of specialized bariatric vitamins that are designed to be gentle on your digestive system while providing the essential nutrients you need after surgery.
Our product line includes everything from bariatric multivitamins—including bariatric multivitamin with iron options—for comprehensive nutritional support, to bariatric vitamins chewable for those who prefer easier-to-take formats. We also carry liquid bariatric vitamin formulas for patients with specific absorption needs or those who have difficulty swallowing pills.
To help meet your protein goals, Bari Life offers a variety of bariatric protein shakes and bariatric protein bars, ideal for maintaining lean muscle mass and supporting metabolic health during recovery. Our delicious bariatric snacks provide healthy, portion-controlled options that can be easily incorporated into your daily routine.
Calcium intake is also important post-surgery, and our bariatric calcium chews are a convenient and tasty way to support bone health. We understand that many patients also face challenges like hair thinning, which is why we offer bariatric vitamins for hair loss that are formulated to target these specific concerns.
Digestive health is another key area of focus. That’s why we include products like our bariatric probiotic, specifically designed to promote a healthy gut microbiome after bariatric procedures.
Visit Bari Life today to explore our complete line of bariatric-specific nutritional products that can support your recovery and help you maintain improvements in both your weight and GERD symptoms following bariatric surgery.
If you want to learn more, why not check out these articles below:
- PCOS and Bariatric Surgery
- Best Bariatric Surgery For Hiatal Hernia
- Malabsorptive Bariatric Surgery
- Bariatric Surgery and Gallbladder
Resources
Clarrett, D. M., & Hachem, C. (2018). Gastroesophageal Reflux Disease (GERD). Missouri Medicine.



What are your tips and tricks to post-bariatric success?